Colonoscopy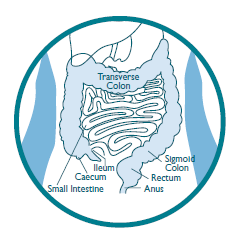
Colonoscopy is a visual examination of the lining of your large bowel (colon) with sedation. A flexible tube (about the thickness of the little finger) is passed through the rectum and around the colon. A small video camera, which can take photos, sends an image onto a video screen. The doctor looks for any abnormalities and if necessary, biopsies (small tissue samples) can be painlessly taken through the colonoscope using tiny forceps. These biopsies are examined under a microscope in the laboratory.
Polyps (abnormal growths of tissue) can be removed with biopsy forceps or cold snaring and large polyps are removed using a diathermy snare. This is done by passing a wire loop, like a lasso, over the polyp. The polyp is cut from the bowel lining using electrical current, which seals the tissue and stops bleeding. This current cannot be felt and causes no pain.
|
During your procedure you will be given sedation. It is important that you arrange for someone to drive you home following your procedure. You are not permitted, by law, to drive yourself. For safety reasons, if you are travelling on public transport, or in a taxi, please arrange for a support person to travel with you.
|